Welcome To Lyme Bytes!
April, 2014- HELLO ALL! I am no longer posting to this blog. For the latest on me and my work, I invite you to subscribe to my NEW blog: www.conniestrasheim.blogspot.com where I share my latest findings on how to heal from chronic illness involving Lyme and other conditions. Thanks!
Greetings and welcome to my Lyme disease blog, a comfy cozy (and sometimes crazy!) place for cutting-edge information, encouragement and insight into the fastest-growing epidemic disease in the United States. In this blog you will find everything from bug-killing strategies to immune system and hormone help, as well as lifestyle and spiritual suggestions for healing from chronic illness involving Lyme disease. The information contained within this blog is based upon my own healing journey and what I have learned over the past eight years as I have been diligently digging and researching my way back to a better state of health. May you find it to be a source of hope, inspiration and wisdom in your own journey towards wellness.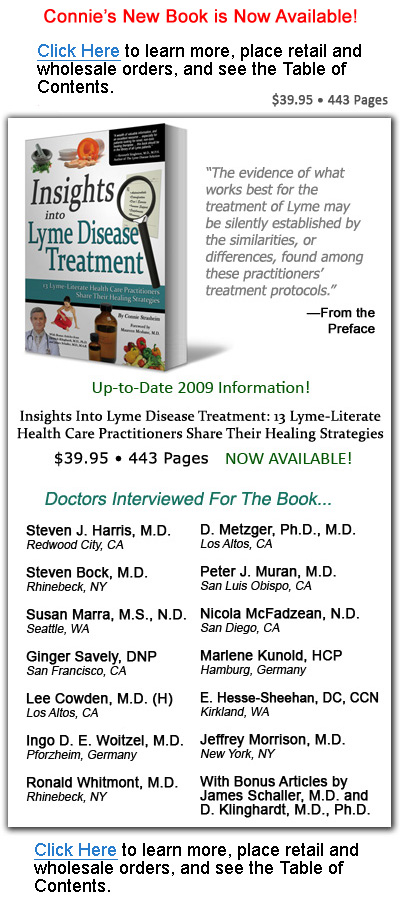
About "Insights Into Lyme Disease Treatment"
About the book:
Published August, 2009
Written by Connie Strasheim
Learn More - Bulk Orders - Table of Contents
Friday, August 08, 2008
Antibiotic Recommendations According to Dr. Harris
From the brief conversation that I had with Dr. Harris, I became interested in his protocol for treating Lyme patients with antibiotics. While I did not arrive at the conference in time to hear Dr. Harris speak, I have summarized here some of the main points of his speech, which were provided in my conference notes. While I personally have not chosen to take antibiotics for my Lyme disease, I know that they have been life-saving for many when a competent and experienced Lyme-literate physician knows how to administer them, and for that reason, I share Dr. Harris' protocol.
For the treatment of chronic Lyme, Dr. Harris advocates starting with a single antibiotic, perhaps doxycycline or minocycline, at 100 mg, for six weeks. After that time, a second antibiotic can be introduced, or the dose of the first one can be increased. Alternatively, cefdinir, (300 mg) cefuroxime (500 mg) or amoxicillin (875 mg), can be used as initial agents. Many chronic Lyme patients will also need parenteral (IV) therapy, but physicians should not begin this until the patient has been on one of the above agents for three or four months. I surmise that this is to not overload the body, since overwhelming herxheimer reactions can occur if high doses of antibiotic are administered in a very sick person. A good parenteral drug of choice, according to Harris, is ceftriaxone (2 grams, for four to seven days a week). He notes that cefotaxime or ampicillin are also effective.
When I first learned that I had Lyme disease, my physician immediately and simultaneously put me on three different antibiotics, including the powerful cell-busting metronidazole. No wonder I didn't last two months on my cocktail! The irremediable insomnia and other debilitating symptoms I experienced as a result (including a monster candida infection that persisted despite other drugs) caused me to discontinue the use of the antibiotics. To this day, I don't regret having stopped them (but for different reasons than those I mention above).
Once a patient has been on a single antibiotic for a number of weeks, Dr. Harris then advocates adding a separate type, that works by a different mechanism and which is in a different class than the first. In his notes, he writes that 500-600 mg of azithromycin or clarithromycin are often good choices if the first antibiotic is a beta-lactam drug. He also mentions that, while tetracyclines and macrolide antibiotics aren't often used in combination because they are both ribosomal inhibitors, in his practice, a combination of the two has proven to be effective. Also, he notes that benzathine PCN 1.2 million units 2-3 times a week is a good adjunct treatment, since it has good CNS penetration.
Finally, cyst-busting drugs such as metronidazole and tinidazole can, and perhaps should, eventually be added into a patient's protocol, and because these must be used in conjunction with a cell-wall active drug, they should be given after a patient has been placed on an antibiotic of this type. He writes that cyst-busters are most effective when pulsed for 2-3 months at a time.
When choosing an antibiotic, it's important to consider the drug's ability to penetrate the central nervous system, along with other factors relating to bacteriocidal activity. The ability of the patient to comply with a regimen should also be taken into account.
During antibiotic therapy, the body must also be protected from harm, and this can be done by regularly monitoring hepatic (liver) and renal (kidney) function, along with blood counts. Probiotics, liver support products, and lymphatic drainage protocol will also help to protect and heal the body. Dr. Harris believes that adverse effects from antibiotics can be limited to less than 5% if the above tests are regularly performed and the patient uses supportive therapies in his/her regimen.
For treatment of babesiosis, he advocates using atovaquone (Mepron) with azithromycin, for four months. If a patient still tests positive for the infection two months after finishing these medications, then the treatment period should be extended to 8-10 months. Alternatively, he mentions that clindamycin may be given to patients, along with quinine and mefloquine. For ehrlichiosis, (ehrlichia) he uses 100 mg of doxycycline or minocycline. For cases that don't respond to these medications, he adds rifampin to the regimen. For bartonella, he advocates 400 mg of gatifloxacin or 500-750 mg of levoflaxin, for four to twelve weeks. Trimethoprim-sulfamethoxazole (Bactrim) can be added, if necessary.
Finally, Dr. Harris notes that some ILADS (read: Lyme-literate) physicians prefer to treat co-infections before borrelia, while others treat with as much overlap as possible. He advocates considering treating Lyme initially for two to three months, then stopping therapy to engage co-infections; however, treating Lyme and babesia simultaneously has proven to be quite successful.



1 comment:
Those antibiotic recommendations works even if I use several doses of my Viagra Online Prescription
Post a Comment